Providing healthcare to vulnerable communities in Yei and Morobo amidst insecurity and funding cuts
In 1 click, help us spread this information :
Mothers with babies strapped on their backs watch from the undergrowth bordering the track as a convoy of cars belonging to international medical organisation Médecins Sans Frontières (MSF) travels with difficulty through the overgrown vegetation. Still and silent, they watch the cars pass by from their hiding places.
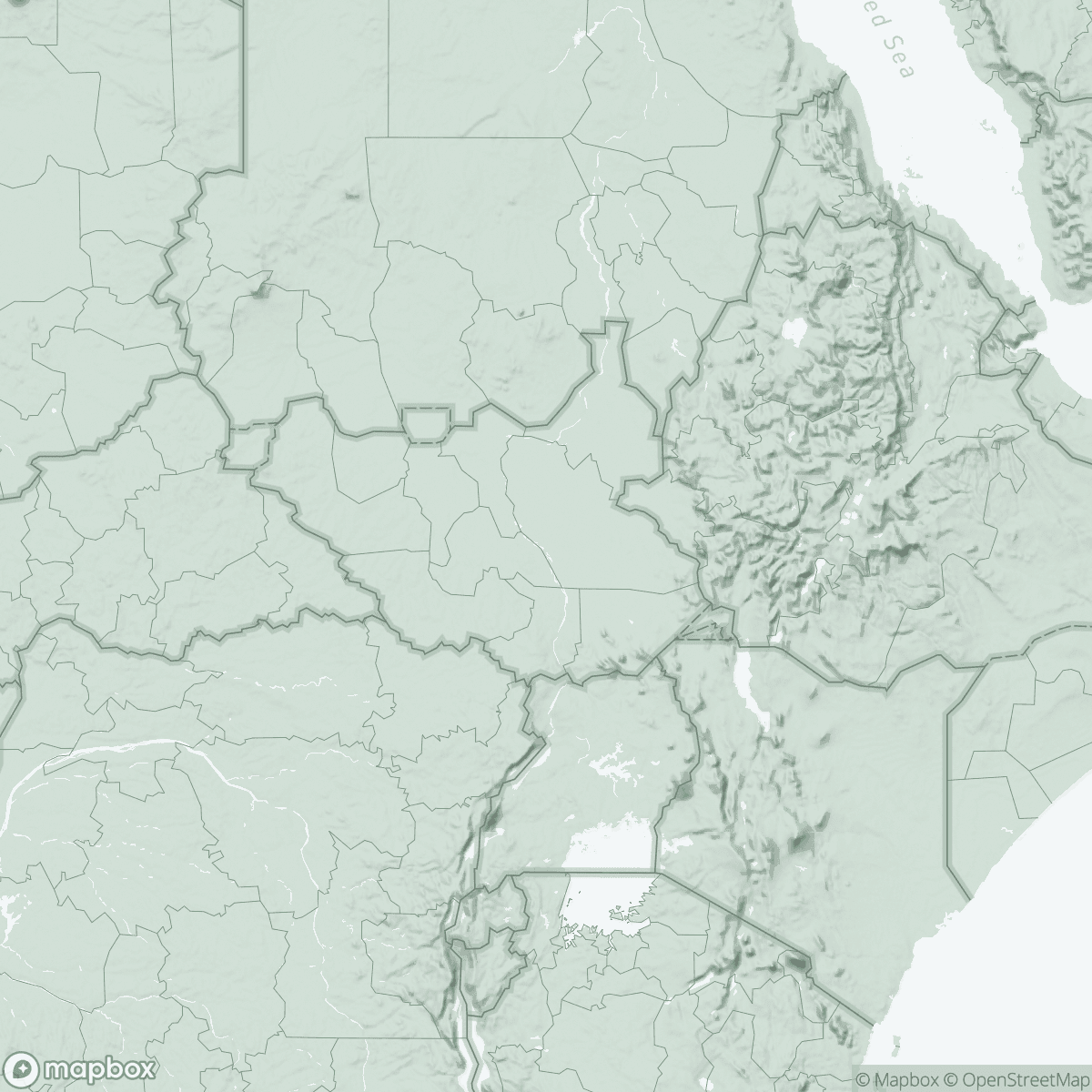
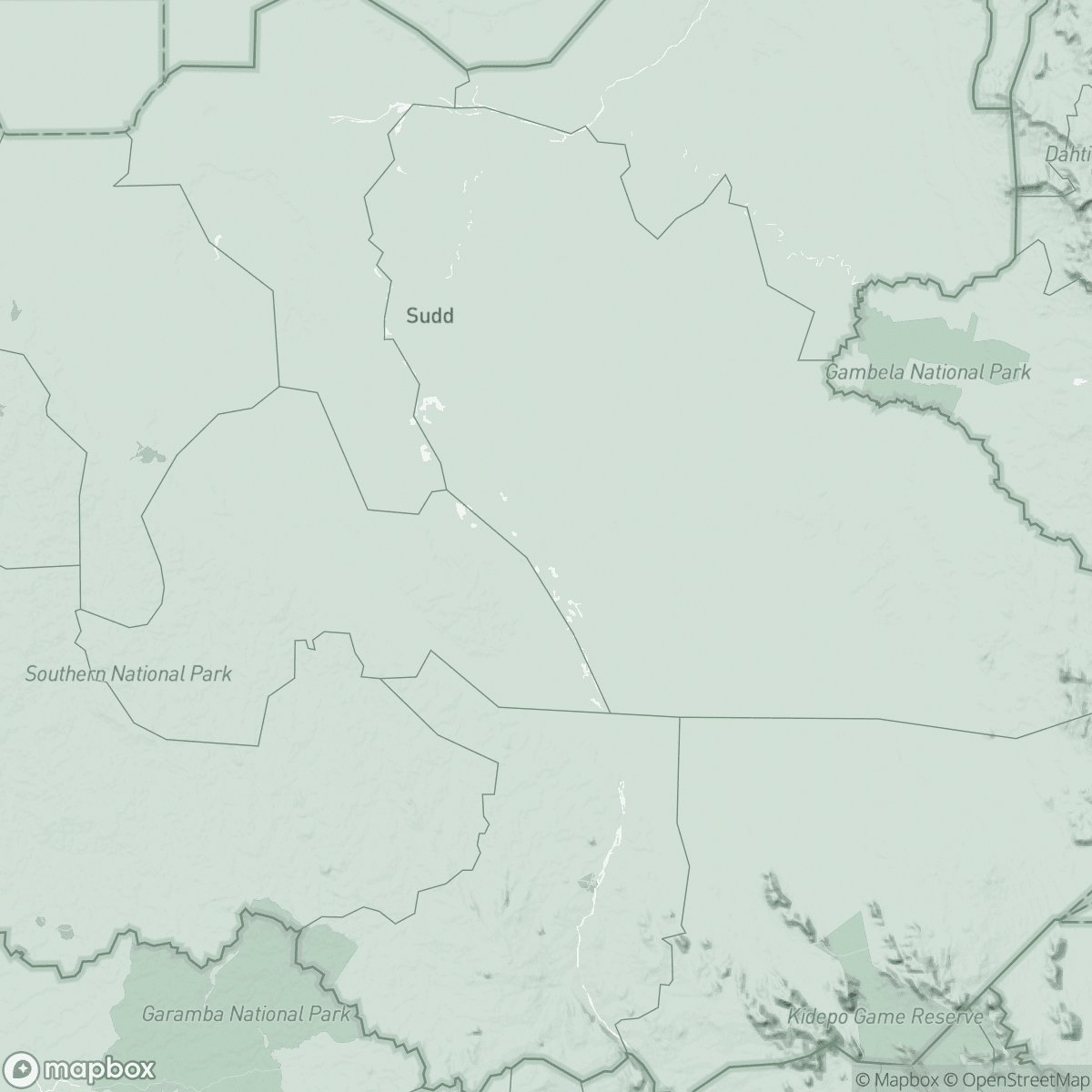
In Yei and Morobo counties, in South Sudan’s Central Equatoria state, a conflict is raging between armed groups; because of the violence, whole communities are regularly displaced from their homes. Many people have fled into the bush in search of safety. Living far from main roads and settlements, people in these communities cannot reach a health facility even if they fall sick.
Even people who are not displaced can have difficulty accessing medical care. In Morobo county, there are just two functioning health facilities for an estimated 150,000 people. To take healthcare closer to vulnerable communities, MSF has two mobile medical teams who run clinics in some of the most remote areas.
“The idea of implementing mobile clinics came to us last year,” says Lubang Alex Charles, MSF outreach nurse activity manager.
Seeing that no other organisations were supporting vulnerable communities, we decided to extend our services to hard-to-reach areas. Depending on the location, we often have to drive three to four hours before setting up the clinic.”
In Yei and Morobo counties, people’s need for healthcare has been increasing since the beginning of this year. MSF teams have seen an influx of returnees from Uganda in response to cuts of international aid on the Ugandan side of the border. Also, with the start of the rainy season, malaria is on the rise, with more than 70 per cent of people in the area testing positive for the disease.
“We see more than 400 patients each day at our mobile clinics,” says Lubang Alex Charles.

We conduct outpatient consultations, provide vaccinations, carry out malaria and malnutrition screenings, and provide antenatal care. We also offer family planning services, care for survivors of sexual violence, mental healthcare, health awareness activities and referrals to hospital for people needing specialist care.”
Given the scale of people’s health needs, MSF teams have also been looking for additional ways to improve their access to basic lifesaving medical care. In Yei county, MSF has been working with community leaders in remote villages to train local people to administer medical care themselves, in an initiative known as ‘integrated community case management’ or ICCM.
“ICCM is a strategy to train, support and supply community health workers,” says MSF’s Amba James Julius, supervisor of the initiative. “It helps provide diagnostic, treatment and referral services for common, treatable and curable illnesses such as malaria, pneumonia and diarrhoea. The community health workers also screen children for malnutrition.”
Joel Lasuba supervises the community health workers in his area, meeting with them every month to check patients’ registers, check on drugs supply and discuss specific cases and challenges:
We face many challenges,” says Lasuba. “We can only treat three illnesses, but people come to us with a lot more sicknesses that we cannot manage. We refer them to Jansuk clinic in Yei town, but they ask for better care in their village. Some cannot travel all the way to the clinic because they are either too weak or too scared.”

Jansuk clinic is one of the few functioning medical facilities in the area, where MSF staff provide basic healthcare. In recent months, the team has seen a decrease in patient numbers as a result of ongoing armed confrontations and related violent incidents, which directly affect local people’s ability to travel on the roads and prevent them from accessing healthcare.
At the same time, humanitarian organisations in Yei and Morobo counties have been downscaling their operations since 2022 due to funding cuts, further threatening access to healthcare for displaced and local communities.
MSF calls for a concerted effort by humanitarian organisations and international donors to ensure access to lifesaving care for all in this conflict-hit region of South Sudan.