Accueil

Nous sommes
Médecins Sans Frontières.
Neutres. Indépendants. Impartiaux.
Depuis plus de 50 ans, nos équipes interviennent auprès des populations exclues des soins de santé.
98% de nos ressources sont d'origine privée. Grâce à vous, nous pouvons agir.
Nous intervenons dans plus de 70 pays
Médecins Sans Frontières est présente dans plus de 70 pays dans le monde. Nous sommes guidés par l'impact, et non par la visibilité médiatique. Nous allons là où nos équipes sur le terrain peuvent faire la différence la plus significative.

Ce que nous faisons grâce à vos dons :
pays où nous intervenons
DE CONSULTATIONS EFFECTUÉES
TRAVAILLEURS HUMANITAIRES ENGAGÉS
Médecins Sans Frontières
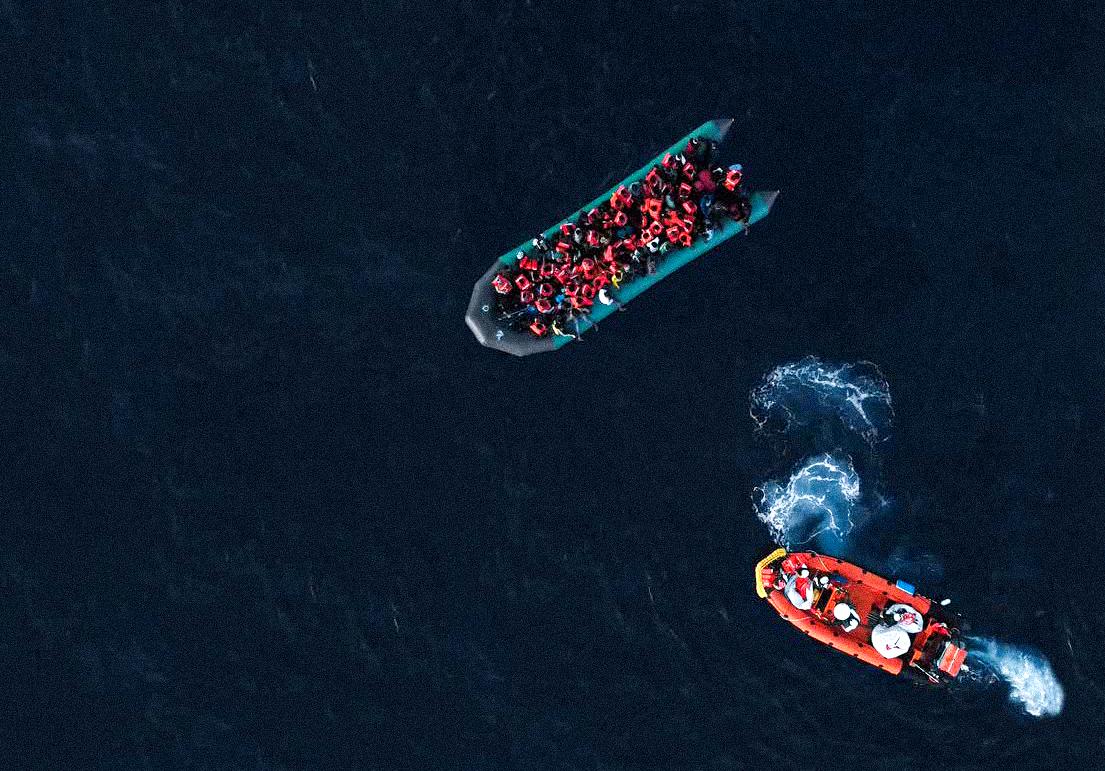
Médecins Sans Frontières (MSF) est l’une des principales organisations humanitaires médicales internationales. Nous fournissons une assistance médicale aux personnes touchées par les conflits, les épidémies, les catastrophes ou l'exclusion des soins de santé dans 74 pays. Depuis plus de 50 ans, nos actions sont guidées par l’éthique médicale et les principes d’impartialité, d’indépendance et de neutralité.
La section luxembourgeoise de MSF a été créée en 1986 et héberge l’unité de recherche opérationnelle, dénommée LuxOR (Luxembourg Operational Research).


Les conditions catastrophiques à Gaza exigent une aide humanitaire massive et urgente

Ce qu'il reste après les flammes : quatre ans de guerre totale en Ukraine
Comment la participation des jeunes renforce les soins adaptés aux adolescents à Mbare

Soudan : MSF prend en charge 170 personnes blessées par des frappes de drones dans des zones civiles à travers le pays

Sud-Kivu : À Sangé, MSF répond à l'épidémie de choléra la plus forte dans la zone depuis 5 ans

MSF lance une réponse d’urgence à El Obeid, près de l’un des fronts les plus actifs du Soudan

Déplacées et oubliées : les familles du nord-ouest de la Syrie confrontées à des conditions hivernales difficiles

Oubliées entre deux frontières : les besoins critiques des personnes déplacées au Soudan du Sud
Mapathon : vos clics feront la différence le 25 février !

Campagne de vaccination contre la rougeole à El Geneina : une première depuis 2021