Accueil
AVANT QUE L’ANNÉE TOUCHE À SA FIN FAIM : AGISSEZ CONTRE LA MALNUTRITION

Nous sommes
Médecins Sans Frontières.
Neutres. Indépendants. Impartiaux.
Depuis plus de 50 ans, nos équipes interviennent auprès des populations exclues des soins de santé.
98% de nos ressources sont d'origine privée. Grâce à vous, nous pouvons agir.
Grâce à vous
Neutralité, indépendance, impartialité, ces 3 principes vous les connaissez sans doute, ce sont ceux qui guident l’action de Médecins Sans Frontières et ils ne pourraient être respectés sans le rôle fondamental des donateurs.
Oui, grâce à vous, MSF peut agir auprès de celles et ceux qui en ont besoin, partout, sans distinction de race, de religion ou d’appartenance ethnique, et sans aucune discrimination !
C'est dans ce contexte, que nous avons lancé notre dernière campagne, « Grâce à vous », soulignant l’importance du rôle des donateurs comme maillon essentiel de notre impartialité, neutralité et indépendance.

Nous intervenons dans plus de 70 pays
Médecins Sans Frontières est présente dans plus de 70 pays dans le monde. Nous sommes guidés par l'impact, et non par la visibilité médiatique. Nous allons là où nos équipes sur le terrain peuvent faire la différence la plus significative.

Ce que nous faisons grâce à vos dons :
pays où nous intervenons
DE CONSULTATIONS EFFECTUÉES
TRAVAILLEURS HUMANITAIRES ENGAGÉS
Médecins Sans Frontières
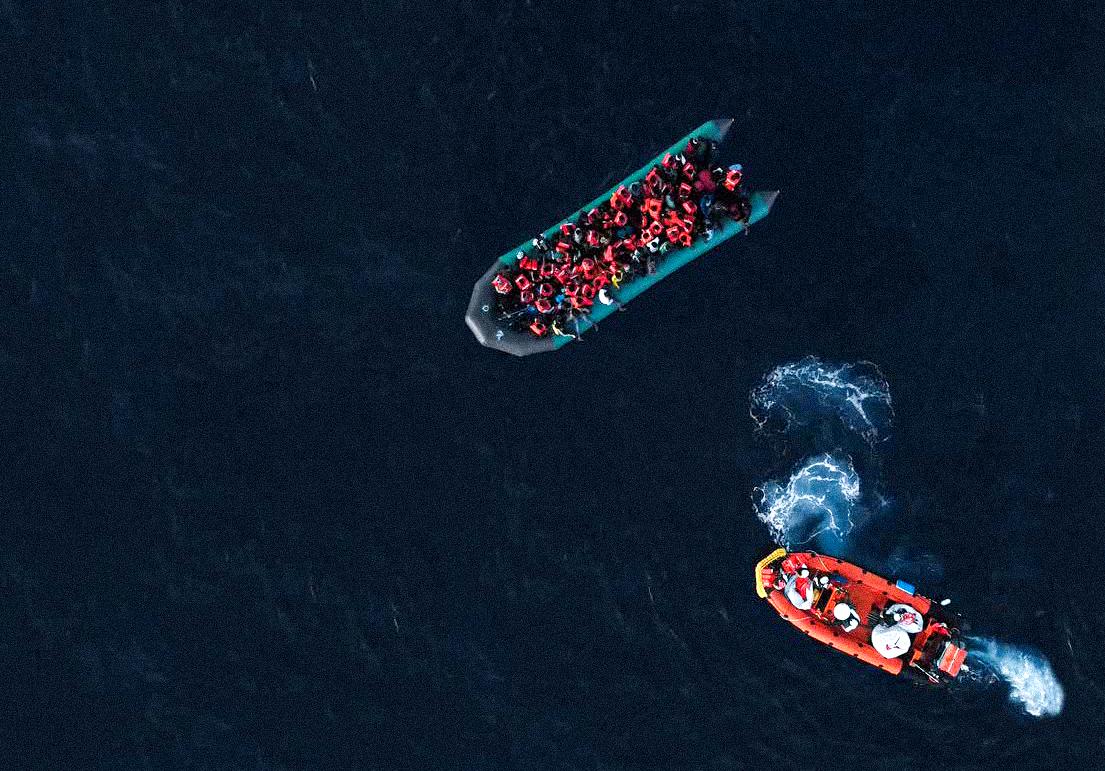
Médecins Sans Frontières (MSF) est l’une des principales organisations humanitaires médicales internationales. Nous fournissons une assistance médicale aux personnes touchées par les conflits, les épidémies, les catastrophes ou l'exclusion des soins de santé dans 74 pays. Depuis plus de 50 ans, nos actions sont guidées par l’éthique médicale et les principes d’impartialité, d’indépendance et de neutralité.
La section luxembourgeoise de MSF a été créée en 1986 et héberge l’unité de recherche opérationnelle, dénommée LuxOR (Luxembourg Operational Research).


À l’ONU, MSF dénonce la montée des violences et la détresse sanitaire dans l’est de la RDC
Perspective de santé mentale en Cisjordanie : « Les Palestiniens se préparent à la perte »

MSF soutient l'évacuation de 13 enfants supplémentaires gravement blessés de Gaza vers la Suisse

Soudan du Sud : des vies menacées par l’effondrement des soins de santé alors que la violence s’intensifie

Projet Couffo, Bénin : Une approche participative pour réduire la morbidité et mortalité maternelle et néonatale

Un centre de santé de MSF touché lors d'une frappe aérienne au Soudan du Sud
RDC : MSF a lancé deux opérations d'urgence à Fizi, Sud-Kivu
Des soins vitaux pour les enfants dans le nord de l'Afghanistan
Fournir des soins médicaux aux populations égyptienne et soudanaise à Assouan
MSF Luxembourg s’engage auprès des jeunes vivant avec le VIH